Tags
BEIR, blindness, cancer, cataract surgery, cataracts, comment, exposure to ionizing radiation, eye protection, eyesight, glasses, ICRP, ionizing radiation, lens, Linear No-Threshold, linear no-threshold dose, medical industry, no-threshold, NRC, nuclear energy, nuclear facilities, nuclear power, opacities to the eye, radiation, radiation dangers, radiation safety, radiology, safety standards, seeing impairment, standards, surgery, US NRC, x-rays
Click to access EPA_SW_FS_EyeDamage_v7_508_RELEASE.PDF
Recent studies have suggested a “no-threshold” dose for cataracts from radiation exposure to the lens of the eyes among radiology and nuclear workers. Is this a surprise? It involves more dangerous ionizing radiation than UV rays, as can be seen on the diagram above. And, when was the last time you heard a medical or governmental recommendation to wear your UV protective sunglasses for only part of the time that you are in the sun? UV protection sunglasses have been recommended for several decades. And, initially they weren’t cheap. But, everyone was told to buy them and use them. No one said that you can expose your eyes for a few hours or years, and then put on the glasses (or hat. [1]) But, this is the same sort of “reasoning” used by the nuclear industry and the so-called protection agencies-organizations, when they pretend that there is a safe dose of radiation to the eyes, and, worse, that huge doses are safe.
The US NRC “standard” for worker eyes is a whopping 150 mSv per year. Recall that, according to BEIR VII, 100 mSv gives an approximate 1% exposure induced cancer risk (1,000/100,000).
Protective eyewear, and other shielding, is available and the cost appears as cheap or cheaper than cataract surgery. So, simply from a financial perspective, the nuclear industry, and those using x-rays in their businesses, are externalizing the cost upon individuals, insurance companies and the taxpayer, when they expose worker eyes.
US NRC Comment Deadline on “Radiation Protection” is today 22 June 2015, 11.59 pm (one minute to midnight) NY-DC (ET). Comment here: http://www.regulations.gov/#!documentDetail;D=NRC-2009-0279-0098 (Remember to put the ID number on your comment: NRC-2009-0279-0098) The original list of questions to be answered is found here: https://www.federalregister.gov/articles/2014/07/25/2014-17252/radiation-protection Comment can be anonymous and it can be short. (If it is too long you will have to upload a pdf document.) Take a screen shot of your comment for the record. The purpose of comment is that it is supposed to be public record. The US NRC ignores this at their own risk from a legal perspective.
One of the questions is whether or not to bring worker eye exposure to radiation down (along with overall worker exposure) to 20 mSv per year, averaged over 5 years with no more than 50 mSv in one year. Currently the US NRC limit for the eyes of those who work with ionizing radiation is 150 mSv. The overall workers exposure limit is 50 mSv per year.
According to the US FDA, and others, “More recent studies suggest that the lowest cataractogenic dose in people is much less than these values, is statistically compatible with no threshold at all, and that increasing dose is associated with an increasing prevalence of cataracts.” (USFDA)
In fact, evidence of a no-threshold effect was reported in animals in the 1970s, according to ICRP 118 (pp. 121-122). The ICRP gloss over this no-threshold so that they can keep the eye dose at 20 mSv per year to match their proposed body dose. It is easy to miss in their over 300 page long document.
Ionizing radiation has been known to cause cataracts for a very long time. The issue, as seen by the US NRC-ICRP – nuclear industry, appears to be how many years can a person see adequately to do their work without surgery – not quality of life or vision. Since the cataracts occur late in life they appear to consider it not their problem.
Cataract surgery is not about removing the cataracts, as many people think. It’s about removing the lens and putting a fake lens which can never be exactly like your real, natural lens. So, post cataract surgery people have to get glasses, even if they didn’t have glasses before. Generally it is considered safe, though the “Health Physics Society” comment points out that some people actually die subsequent to surgery.
This discusses some of the risks: https://www.dhs.wisconsin.gov/blind/eyediseases/cataract-surgery.htm
In 1977, 300 mSv of radiation to the eyes was suggested by the ICRP. In 1991 they dropped it to 150 mSv and now they decided they were wrong and suggest 20 mSv per year (100 mSv for 5 years). In other words 15 x more radiation to the eyes was recommended in 1977 compared to 2012. http://pbadupws.nrc.gov/docs/ML1408/ML14084A341.pdf
The US NRC, as a leading cog in the nuclear industry, apparently wants to keep this 150 mSv dose to the eye lens (as does Exelon and probably the rest of the nuclear industry). They also want to keep the overall dose at 50 mSv per year. Exelon, and one or more others, whine that the body dose won’t match the eye dose, whereas if the body dose is brought down from 50 mSv to 20 mSv, then it would match the eye dose of 20 mSv.
They don’t give a damn that “The lens of the eye is one of the most radiosensitive tissues in the body (Brown, 1997; Ainsbury et al., 2009). When the radiosensitivity of various eye tissues is compared, detectable lens changes are noted at doses between 0.2 and 0.5 Gy, whereas other ocular pathologies in other tissues occur after acute or fractionated exposures of between 5 and 20 Gy” (ICRP, 118, p. 117) On ICRP 118, p. 23 they explain the use of Gy vs Sv. (see more on this in note [2]) For purposes of this comment period it is important to use mSv, since it includes important weighting factors, by definition. Furthermore, Sieverts is the appropriate unit for stochastic effects (randomly induced effects with no threshold), which many now think that cataracts may be.
Thus, the detectable lens changes are at between 200 and 500 mSv, but this may be cumulative over time. In 16 months at 150 mSv a worker reaches the 200 mSv. At the ICRP recommended 20 mSv it would be reached in 10 years.
A comment submitted by the “Health Physics Society” to the US NRC discusses the cost of eye protection: “Prescription eyewear containing lead glass and side shields generally cost in excess of $300 per individual and would need to be replaced every 12 to 24 months as the individual refraction prescription changes with age. A single additional in-room shield generally costs in excess of $5,000. The dollar figures are approximate and have not been validated.” [3]
The total average cost of cataract surgery is approximately $6,460 for both eyes (2013) based on a report commissioned by AllAboutVision. com. For a “high-tech” lens the price would be 8,700$ for both eyes. Thus, the financial cost of protective eye-ware over worker career, or additional shielding, appears equivalent to or less than surgery. Furthermore, the “Health Physics Society” points out that some people do appear to die from cataract surgery. It is not so innocuous as one is led to believe.
In “Mayo Clinic. ‘Cataract surgeries on the rise as boomers age, raising access, cost issues.’ ScienceDaily. ScienceDaily, 9 October 2013, one learns that cataracts affect at least 22 million people in the US, and cost almost $7 billion to correct each year. Elsewhere you can read that people in their 40s and 50s are now having cataract surgery. For those over 65 the US taxpayer picks up the tab; for those under 65, the individual or the insurance.
The direct medical costs of cataracts are $6.8 billion annually, according to the EPA
Click to access EPA_SW_FS_EyeDamage_v7_508_RELEASE.PDF
According to the ICRP 118: “if there is zero threshold for radiation cataracts, current radiation safety standards for workers as well as the general population may be inadequate. It is therefore essential for the risk-assessment community to know whether visually disabling cataract formation is a stochastic response to radiation;… At a microscopic level, radiation damage to single lens epithelial or fibre cells probably results in small localised changes in lens transparency, and is therefore a stochastic event. Support for this hypothesis is provided by the linear relationship between radiation dose and the number of small, discrete dots in the posterior lens cortex of animals exposed to either low- or high-LET radiation (Di Paola et al., 1972) (Fig. 2.8). Di Paola et al. suggested that accumulation and coalescence of these micro-opacities results in populations of damaged lens fibre cells that form larger lens defects, eventually resulting in a clinical opacity.” (ICRP 118, p. 121-22) Emphasis our own. Note that Di Paola’s work was in the 1970s! It was over 40 years ago!
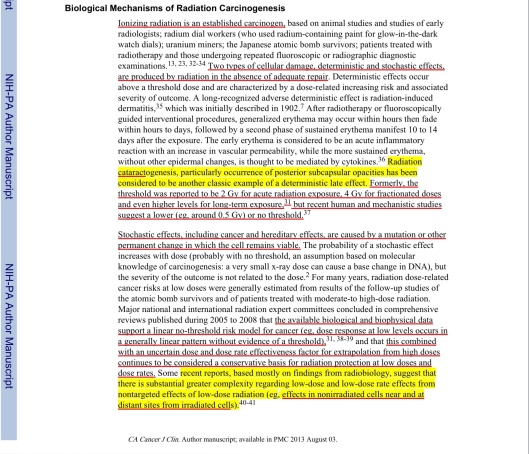
According to the US National Cancer Institute-National Institute of Health:
“Radiation cataractogenesis, particularly occurrence of posterior subcapsular opacities has been considered to be another classic example of a deterministic late effect. Formerly, the threshold was reported to be 2 Gy for acute radiation exposure, 4 Gy for fractionated doses and even higher levels for long-term exposure, but recent human and mechanistic studies suggest a lower (eg, around 0.5 Gy) or no threshold.” Linet, Martha S. et al. “Cancer Risks Associated with External Radiation From Diagnostic Imaging Procedures.” CA: a cancer journal for clinicians 62.2 (2012): 75–100. PMC. Web. 22 June 2015.(Emphasis added) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3548988/ Once again, this 0.5 Gy is equivalent to 500 mSv (500 mGy).
“…recent re-evaluation of current lens occupational exposure guidelines, and a proposed lowering of the presumptive radiation cataract threshold to 0.5 Gy/year and the occupational lens exposure limit to 20 mSv/year, regardless of whether received as an acute, protracted, or chronic exposure. Experimental animal studies support these conclusions and suggest a role for genotoxicity in the development of radiation cataract. Recent findings of a low or even zero threshold for radiation-induced lens opacification are likely to influence current research efforts and directions concerning the cellular and molecular mechanisms underlying this pathology. Furthermore, new guidelines are likely to have significant implications for occupational and/or accidental exposure, and the need for occupational eye protection (e.g. in fields such as interventional medicine).” Ann ICRP. 2012 Oct-Dec;41(3-4):80-97. “Radiation cataract“, by Kleiman NJ http://www.ncbi.nlm.nih.gov/pubmed/23089007
“The possible stochastic nature of cataracts and of CVD renders the boundary between tissue reactions and stochastic effects vague and may call for a new concept for the classification of radiation effects” (“Emerging issues in radiogenic cataracts and cardiovascular disease”
Journal of Radiation Research, 2014, 55, 831–846 Nobuyuki HAMADA et. al. http://jrr.oxfordjournals.org/content/55/5/831.full (This interesting and useful paper was funded by Japan Nuclear Interests.)
From the UK gov: “the HPA endorses the conclusion reached by the ICRP in their 2011 statement that the equivalent dose limit for the lens of the eye should be reduced from 150 to 20 mSv per year, averaged over a five year period, with no year’s dose exceeding 50 mSv.” J Radiol Prot. 2012 Dec;32(4):479-88. “Radiation-induced cataracts: the Health Protection Agency’s response to the ICRP statement on tissue reactions and recommendation on the dose limit for the eye lens.” Bouffler S, Ainsbury E, Gilvin P, Harrison J.
According to the US FDA re Cataracts:
“More recent studies suggest that the lowest cataractogenic dose in people is much less than these values, is statistically compatible with no threshold at all, and that increasing dose is associated with an increasing prevalence of cataracts.9,10,11,12
9 E. Nakashima, K. Neriishi, and A.Minamoto, “A reanalysis of atomic-bomb cataract data, 2000–2002: a threshold analysis,” Health Phys. Vol. 90, pp. 154–160, 2006.
10 Kazuo Neriishi et al., “Postoperative Cataract Cases among Atomic Bomb Survivors: Radiation Dose Response and Threshold,” Radiat. Res. Vol. 168, pp. 404-408, 2007.
11 Gabriel Chodick, “Risk of Cataract after Exposure to Low Doses of Ionizing Radiation: A 20-Year Prospective Cohort Study among US Radiologic Technologists,” American Journal of Epidemiology Vol. 168, No. 6, pp. 620-631, 2008.
12 E. A. Ainsbury et al., “Radiation Cataractogenesis: A Review of Recent Studies,” Radiation Research Vol. 172, pp. 1-9, 2009.” http://www.fda.gov/Radiation-EmittingProducts/RadiationSafety/RadiationDoseReduction/ucm232550.htm
“Radiation cataractogenesis: a review of recent studies. Radiat Res. 2009 Jul;172(1):1-9
Ainsbury EA, Bouffler SD, Dörr W, Graw J, Muirhead CR, Edwards AA, Cooper J.
Abstract
The lens of the eye is recognized as one of the most radiosensitive tissues in the human body, and it is known that cataracts can be induced by acute doses of less than 2 Gy of low-LET ionizing radiation and less than 5 Gy of protracted radiation. Although much work has been carried out in this area, the exact mechanisms of radiation cataractogenesis are still not fully understood. In particular, the question of the threshold dose for cataract development is not resolved. Cataracts have been classified as a deterministic effect of radiation exposure with a threshold of approximately 2 Gy. Here we review the combined results of recent mechanistic and human studies regarding induction of cataracts by ionizing radiation. These studies indicate that the threshold for cataract development is certainly less than was previously estimated, of the order of 0.5 Gy, or that radiation cataractogenesis may in fact be more accurately described by a linear, no-threshold model. http://www.ncbi.nlm.nih.gov/pubmed/19580502
Part of the Health Physics Society Comment Submitted to the USNRC:
“Q2–6: What are the potential operational impacts of lowering the annual occupational dose to the lens of the eye from the current NRC regulatory standard of 150 mSv to 50 mSv? • Would a reduction in the occupational dose limit for the lens of the eye require changes in programs, procedures, practices (e.g., increased use of protective eyewear), or in-room shielding? If so, please describe these changes, including any potential implementation and operational costs.
Response: It is likely that such a reduction would require the increased use of protective eyewear and/or shields in a medical setting. Prescription eyewear containing lead glass and side shields generally cost in excess of $300 per individual and would need to be replaced every 12 to 24 months as the individual refraction prescription changes with age. A single additional in-room shield generally costs in excess of $5,000. The dollar figures are approximate and have not been validated…. HPS wishes to bring the following information to the attention of NRC: • Cataract surgery is generally viewed as an ophthalmological procedure with relatively low morbidity and mortality but with considerable overall economic costs; e.g., consuming greater than 40% of overall U.S. ocular disease expenditures (approximately $5.1 billion) in 1999.7 Nevertheless, available data suggest mortality following cataract surgery is on the order of 0.1% 8,9 and that morbidity, defined both from an ophthalmological as well as medical standpoint, is considerably higher. • Of equal import, prior to a documented clinical need for cataract surgery, there may be accompanying progressive decreases in visual acuity, contrast sensitivity, and visual function that may negatively impact worker performance.” (HPS comment submission May 2015 [3] link at bottom)
The US NRC is ignoring the “findings” of the ICRP 118 regarding cardiovascular and cerebrovascular disease and only discussing the new ICRP “findings” re cataract risk, which the NRC doesn’t seem very interested in implementing:
IRCP 118, Summary:
“ICRP Statement on Tissue Reactions / Early and Late Effects of Radiation in Normal Tissues and Organs – Threshold Doses for Tissue Reactions in a Radiation Protection Context ICRP Publication 118 Ann. ICRP 41(1/2), 2012, by F.A. Stewart, A.V. Akleyev, M. Hauer-Jensen, J.H. Hendry, N.J. Kleiman, T.J. MacVittie, B.M. Aleman, A.B. Edgar, K. Mabuchi, C.R. Muirhead, R.E. Shore, W.H. Wallace
Abstract – This report provides a review of early and late effects of radiation in normal tissues and organs with respect to radiation protection. It was instigated following a recommendation in Publication 103, and it provides updated estimates of ‘practical’ threshold doses for tissue injury defined at the level of 1% incidence. Estimates are given for morbidity and mortality endpoints in all organ systems following acute, fractionated, or chronic exposure. The organ systems comprise the haematopoietic, immune, reproductive, circulatory, respiratory, musculoskeletal, endocrine, and nervous systems; the digestive and urinary tracts; the skin; and the eye.
Particular attention is paid to circulatory disease and cataracts because of recent evidence of higher incidences of injury than expected after lower doses; hence, threshold doses appear to be lower than previously considered. This is largely because of the increasing incidences with increasing times after exposure. In the context of protection, it is the threshold doses for very long follow-up times that are the most relevant for workers and the public; for example, the atomic bomb survivors with 40–50 years of follow-up. Radiotherapy data generally apply for shorter follow-up times because of competing causes of death in cancer patients, and hence the risks of radiation-induced circulatory disease at those earlier times are lower.
…. for reactions manifesting very late after low total doses, particularly for cataracts and circulatory disease, it appears that the rate of dose delivery does not modify the low incidence. This implies that the injury in these cases and at these low dose levels is caused by single-hit irreparable-type events. For these two tissues, a threshold dose of 0.5 Gy is proposed herein for practical purposes, irrespective of the rate of dose delivery, and future studies may elucidate this judgement further. “ICRP, 2012 ICRP Statement on Tissue Reactions / Early and Late Effects of Radiation in Normal Tissues and Organs – Threshold Doses for Tissue Reactions in a Radiation Protection Context. ICRP Publication 118. Ann. ICRP 41(1/2).”
http://www.icrp.org/publication.asp?id=ICRP%20Publication%20118
Notes
[1] Recent research has suggested that wearing hats to shade the eyes offers the best protection from sun damage to the eyes.
[2] For purposes of this comment period it is important to use mSv, since it includes important weighting factors, by definition. The ICRP states that Gray must be multiplied by RBE (Relative Biological Effectiveness) for alpha emitters for “deterministic” effects, which makes it the same as Sieverts, anyway, which they claim is only for “stochastic” (random) effects. For instance 1 mGy of alpha would be 20 mSv. They recommend using RBE x mGy which would make alpha emitters 20 mGy, but this leaves it wide open for dangerous error by the often stupid and often evil cogs at the US NRC. The US NRC is also asking the question in rems or sieverts. Furthermore, Sieverts is the appropriate unit for stochastic effects, which they now think that damage to the eye may be. Using Gray without weighting factors could lead to twenty times more radiation than considered “safe”!
[3] Health Physics Society Public Comment Submission Link: http://www.regulations.gov/contentStreamer?documentId=NRC-2009-0279-0131&attachmentNumber=1&disposition=attachment&contentType=pdf
Linet, Martha S. et al. “Cancer Risks Associated with External Radiation From Diagnostic Imaging Procedures.” CA: a cancer journal for clinicians 62.2 (2012): 75–100. PMC. Web. 22 June 2015.(Emphasis added-US Gov-Public Domain journal) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3548988/ Once again, this 0.5 Gy is equivalent to 500 mSv (500 mGy).


You must be logged in to post a comment.