Tags
Atomic Bombing, cataracts, Chernobyl, children, CT scans children, dangers of ionizing radiation, Hiroshima, Nagasaki, nuclear accident, nuclear industry, nuclear power, radiation, radiation induced cataracts
“What is a cataract?
A cataract is a clouding of the lens in the eye that affects vision.” http://www.nei.nih.gov/health/cataract/cataract_facts.asp
Vision blurred by cataracts

Both images by Marcela via wikimedia
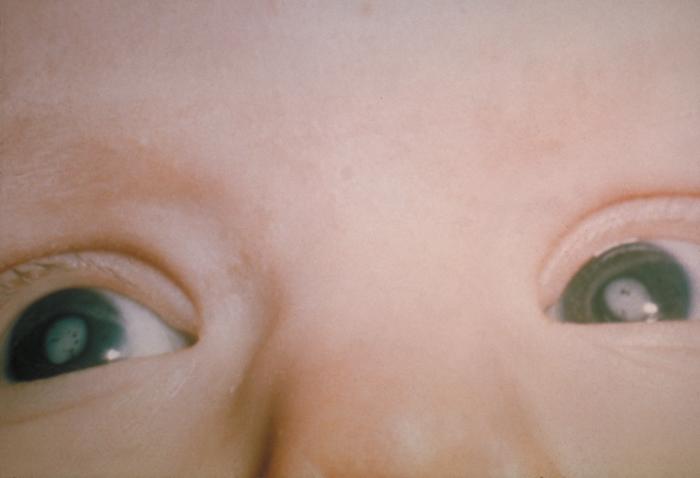
Cataracts in a child, US CDC [1]
Links, which may be of help, for those who want detailed understanding of sievert vs. gray, radiation measurements:
Sv is sievert: http://en.wikipedia.org/wiki/Sievert
Gy is Gray: http://en.wikipedia.org/wiki/Gray_(unit)
http://en.wikipedia.org/wiki/Committed_dose http://en.wikipedia.org/wiki/Equivalent_dose http://en.wikipedia.org/wiki/Effective_dose_(radiation)
From “European Commission Directorate-General for Energy, Directorate D – Nuclear Safety and Fuel Cycle Radiation Protection, Meeting of the Group of Experts established under Article 31 of the Euratom Treaty, Luxembourg, 19–21 November 2012, Summary Report, Annex 1“:
(page 12) “Radiation induced cataracts and age at exposure
Review of publications
Working Party “Research Implications on Health and Safety Standards” of the Article 31 Group of Experts
During the EU Scientific Seminar held in Luxembourg on 17 October 2006 about “New Insights in Radiation Risk and Basic Safety Standards”, Norman J. Kleiman, Director of the Eye Radiation and Environmental Research Laboratory in the Columbia University, reviewed the new available evidence regarding radiation-induced cataracts. Kleiman concluded that the evidence to date pointed to a dose threshold no greater than 700 mGy, which challenged the ICRP guidelines, based at this time on postulated threshold doses of 5 Sv (equivalent dose) for detectable opacities and 8 Sv for visual impairment (cataract) in conditions of highly fractionated or protracted exposure (adult population) (ICRP 60, annexe B, p 103, table B-1), with corresponding figures for single acute exposures of 0.5-2 and 5 Sv. The dose limit for the lens of the eye for members of the public was based on “an arbitrary reduction factor of 10” (ICRP 60, p 46, 194). Moreover, Kleiman reported new observations that are consistent with the absence of a dose threshold. Although the mechanism of radiation induced cataracts is not known precisely, genomic damage resulting in altered cell division, transcription and/or abnormal lens fibre cell differentiation should be considered to be the salient injury, rather than cell killing. For this reason, the classification of cataracts as a deterministic effect was called into question. Since the 2006 EU Seminar, a lot of new evidence confirming Kleiman’s conclusions has been published and reviewed (among others by the WP RIHSS). Based on the work of its Task Group on early and late non-cancer effects of radiation in normal tissues and organs, ICRP finally issued a Statement on tissue reactions on 21 April 2011. According to this Statement, “the threshold in absorbed dose for the lens of the eye is now considered to be 0.5 Gy” and, “for occupational exposure in planned exposure situations, the Commission now recommends an equivalent dose limit for the lens of the eye of 20 mSv in a year, averaged over defined periods of 5 years, with no single year exceeding 50 mSv”.
In the current EC proposal for new BSS, based on the above-mentioned ICRP statement, the dose limit for the lens of the eye is lowered for exposed workers (20 mSv/y). Regarding dose limits for the lens of the eye for members of the public (including infants and children), ICRP did not propose anything explicitly in its statement but, from oral explanations of the ICRP secretary and of ICRP members, it appears that no change was considered necessary. This issue was discussed during a meeting of the Article 31 Group of Experts and the WP RIHSS was asked to review the literature data concerning specifically the possible role of the age at exposure on the risk of radiation-induced cataracts. With this in view, Serena Risica gathered together all the possibly relevant publications. Based on this and on the data found in other recent reviews, the WP RIHSS tried to summarize in this document the published information specifically in relation with the risks of radiation-induced lens defects after exposure at young age. While not highlighting particularly the age at exposure effect, the ICRP draft report on “Early and late effects of radiation in normal tissues and organs: threshold doses for tissue reactions and other non-cancer effects of radiation in a radiation protection context”, contains a comprehensive compilation and a
page 13
discussion of most of the relevant publications and will then be used as one of the basic sources in this document. Work currently in progress in UNSCEAR on “Effects of radiation exposure on children” has also be taken into account.
Regarding chronic irradiation, minor posterior subcapsular opacities were reported after only a few years follow up in children in the Chernobyl area with an excess among those in the exposed areas compared with the unexposed area (Day et al., 1995). There was a small but statistically significant increase in the incidence of sub-clinical posterior subcapsular lens changes (3.6%), greatest among males 12-17 years old at the time of examination, in ~1,000 exposed children, compared to a matched population of ~800 unexposed subjects. Estimates of cumulative dose ranged from 29-86 mSv.” The ICRP draft report noted, however, that dose estimates contain large inherent uncertainties; for example, individual dose estimates were not determined but instead based on recorded environmental exposure levels. The authors also noted that the ophthalmologists were not blinded as to the identity of the exposed and unexposed subjects as exposed children were mainly defined by the environmentally contaminated villages where they currently lived. To minimise potential observer bias, the study included examination by two independent ophthalmologists. The authors also noted that population migration after the disaster may have affected the results in unknown ways as the exposed population was selected from those who resided in formerly contaminated areas at the time of the ophthalmic examinations and thus did not represent a random sampling of all children exposed at the time of the accident. On the other hand, the ICRP draft underlined that the presence of posterior subcapsular defects of a type consistent and characteristic of ionising radiation exposure and not normally found in a paediatric population is suggestive of cause and effect. If additional support for continued ophthalmological examinations and better dose reconstruction in this cohort is forthcoming, a well-designed epidemiological study has the potential to provide additional statistical support for these findings.
There were some (often not translated and not referenced in Pubmed) publications from Russian, Ukrainian or Byelorussian authors related to cataracts in children (for ex. Arinchin, 1998, or Shubik VM and Kvasova MD, 1996), with sometimes unusual information, as the detection of antibodies against antigens of the lens in persons living in areas contaminated after the Chernobyl accident.
A study of a paediatric population accidentally exposed while living in 60Co-contaminated apartment was conducted in Taiwan. It allowed evaluating quantitatively the lenticular changes in a young population exposed to chronic low-dose-rate gamma radiation (Chen et al., 2001). A total of 114 exposed individuals participated in a thorough ophthalmological examination in 1998. The lenticular opacities were evaluated by slit-lamp biomicroscopy after full pupil dilatation and were scored by the Lens Opacities Classification System III (LOCS III) and a modified subclinical minor lenticular focal defects system. These individuals were further divided into those less than 20 years old, those between 20 and 40 years old, and those more than 40 years old to evaluate the effects of age. Mean cumulative exposure of 170 mGy was noted in this population although doses ranged from 1-1,200 mGy. A significant dose-dependent increase in the numbers of focal lens defects in those less than 20 years old was demonstrated, while less significant changes were observed in the other two age groups or by the LOCS III scoring. Results suggested that chronic low-dose-rate irradiation might induce minor lenticular changes, especially in lenses of young subjects.
page 14
A recent follow-up of some of these children after a second ophthalmology examination, all still less than 23 years old, indicated that radiation induced lens changes, measured as sub-clinical focal lens defects (FLD), continued to increase in size and number years after relocation from the contaminated site (Hsieh et al., 2010). The progressive nature of such changes five years later, in a paediatric population now removed from the contaminated environment, demonstrates that such radiation induced lens changes may persist and progress with time.
The radiation-induction of lens opacities was evident in adults who were treated as infants (<18 months old) with external X-ray or radium therapy to treat haemangiomas of the head, face or neck (Hall et al., 1999), when compared with a control population of 89 unexposed, age-matched individuals who presented with skin haemangiomas as infants but were not treated with ionising radiation. The LOCS II lens opacification classification criteria was used and lens dose was estimated based on patient treatment records and photographs, type of radiotherapy (flat applicators, type and number of externally placed tubes or needles or X-ray treatments) and experimental lens absorbed dose calculations using a phantom. These individuals were treated between 35 and 54 years earlier and exposed subjects received an average of two treatments with a cumulative mean dose of 0.4 Gy (median 0.2 Gy, maximum 8.4 Gy). Lens opacities of any type were found in 37% of exposed subjects compared to 20% of controls. A dose response relationship was noted, regardless of age at exposure.
Another study of 20 persons 30-45 years after being treated for skin haemangioma in infancy noted pre-cataractous subcapsular lens changes in the eyes on the untreated side of the face, where lens doses were estimated to average 0.1 Gy (Wilde and Sjostrand, 1997). Although the number of cases is limited, this study suggests a very low dose threshold for radiation-induction of cataracts in young children (median age 6 months).
First evidence on an age at exposure effect in Japanese survivors came from the studies of Choshi (Choshi et al, 1983) and Otake (Otake et al, 1992). Later, the study of Minamoto [Minamoto et al, 2004] on 913 individuals, including mostly persons who were younger than 13 years at the time of the bombings, showed a significant increase in cortical and posterior subcapsular cataracts. Nakashima (Nakashima et al, 2006) tested the fitness of the threshold model and the age at exposure effect in a reanalysis of practically the same data as in Minamoto's study. The results suggested that, in 730 atomic-bomb survivors, we cannot conclude there is a threshold for cortical cataract and posterior sub-capsular opacity (lower 90% CI <0.0). Threshold dose point estimates were 0.6 Sv (90% CI, <0.0-1.2 Sv) and 0.7 Sv (90% CI, <0.0-2.8 Sv) for cortical cataract and posterior sub-capsular opacity, respectively. In addition, there was a clear increase in the dose–effect odds ratio for posterior subcapsular opacity with decreasing age at exposure (p <0.001). The OR/Sv was 1.44 at age of exposure of 10 y (95% CI, 1.19-1.73), and this dose effect decreased significantly with increasing age at exposure and could no longer be demonstrated at an exposure age of 30 years.
Further data on the incidence of cataract extractions in the A-bomb AHS cohort have also indicated an age-at-exposure effect (p = 0.006) [Neriishi et al, 2012]. A total of 1,028 persons out of the cohort of 6,066 had a first cataract extraction during 1986–2005. An analysis adjusted for city, gender, diabetes and time since exposure showed that fifty years after exposure, the relative risks at 1 Sv were 1.61, 1.32 and 1.15 for those exposed at ages 10, 20 and 30 years, respectively.
page 15
A recent publication of IRSN (Michel et al, 2011) aims to estimate the eye lens doses of a pediatric population exposed to repeated head CTs. Children treated for a cholesteatoma, who had had at least one CT-scan of the middle ear before their tenth birthday, were included. At the time of the study (mean age: 16 years), the mean number of CT per child was 3. Cumulative mean effective and eye lens doses were 1.7mSv and 168mGy, respectively. This study is worth mentioning as it illustrates that medical exposures of children can easily exceed threshold doses observed in the above mentioned studies.
Paragraph 697 of the ICRP report on “Early and late effects of radiation in normal tissues and organs: threshold doses for tissue reactions in a radiation protection context” (ICRP publication 118, 2012), concludes that “Overall, the general consistency of the collective results for both early lens opacities and advanced cataracts makes a compelling “weight of evidence” judgment that the recommended acute dose threshold for the purposes of radiation protection should be lowered from its current value to a nominal value of 0.5 Sv” but that “this is subject to the caveats that the progressive nature of assessed opacities into cataracts, and the likely greater sensitivity of the lens in children compared to post-adolescents, require further characterization”. Paragraph 698 states that “For fractionated and protracted exposures, the current epidemiological evidence indicates that the threshold is not larger than for acute exposures, although animal data suggest that a higher value might be plausible. For chronic exposure over several to many years, much of the evidence refers to opacities rather than frank cataracts. The uncertainties about progression of opacities into cataracts, and the age at exposure problem mentioned above, make difficult any judgment about dose thresholds for chronic exposures”.
Interesting in this respect is this judgment coming from the recent ICRP publication 118: “Most tissues show a sparing effect of dose fractionation, so that total doses for a given endpoint are higher if the dose is fractionated rather than when given as a single dose. However, for reactions manifesting very late after low total doses, particularly for cataracts and circulatory disease, it appears that the rate of dose delivery does not modify the low incidence. This implies that the injury in these cases and at these low dose levels is caused by single-hit irreparable-type events”.
In a recent publication, Thorne MC concluded that the accumulating radiobiological and epidemiological evidence makes it more appropriate to treat cataract induction as a stochastic rather than a deterministic effect (Thorne, 2012).
In 2009, the German Commission on Radiological Protection (SSK) also reviewed the available data and adopted new recommendations regarding radiation-induced cataracts. The SSK considered that recent epidemiological studies have not demonstrated any threshold value below which damage to the lens of the eye from ionising radiation can be ruled out with certainty and that there is a strong probability that the threshold dose is < 0.8 Gy. According to SSK, the effects of early childhood exposure to radiation merit particular attention.
According to Shore (Shore et al, 2010), a question of importance for radiation protection purposes is the degree to which the risk of radiation associated opacities is modified by age at exposure.
page 16
“Several different studies reported that exposure at an early age confers more risk per unit dose than exposure at a later age, although some human data have not provided support for this.“
For Ainsbury too (Ainsbury 2009), the importance of age at exposure is evident in a number of the studies, and in particular for posterior subcapsular opacities.
Globally, while it is clear that the number of data related to the risk of radiation-induction of cataracts after exposure of children is currently limited, there is growing evidence of an increased risk compared with this related to adult exposures and of low threshold values. The current evidence seems sufficient to be cautious with exposures of children's eyes, as well in the medical field (the cumulative eye lens dose of 3 CT for a child can approach 200 mGy) as in accidental and post-accidental situations. In normal situations, while a recent study of IRSN has shown that sources of eye exposure are currently practically inexistent for children and members of the public, it would be wise to limit eye exposures to a significantly lower level than the level tolerated for exposed workers, for reasons of consistency and taking into account possible future sources within consumer products.
——————————
References
1. EC, New Insights in Radiation Risk and Basic Safety Standards , Proceedings of the EU Scientific Seminar 2006, Radiation Protection 145, Luxembourg, 2007.
2. EC, Recent scientific findings and publications on the health effects of Chernobyl, Radiation Protection 170, Luxembourg, 2011.
3. Day, R., Gorin, M.B., Eller, A.W., 1995. Prevalence of lens changes in Ukrainian children residing around Chernobyl. Health Phys. 68, 632-642.
4. Arinchin, A.N. and Ospennikova, L.A. Lens opacities in children of Belarus affected by the Chernobyl accident (KURRI-KR–21). Imanaka, T. (Ed.). Japan (http://www.rri.kyoto-u.ac.jp/NSRG/reports/kr21/kr21pdf/Arinchin.pdf)
5. Shubik VM, Kvasova MD. Immunological studies on cataracts under conditions of exposure to low-dose radiation. Vestn Oftalmol.1996 Sep-Oct;112(4):21-3 (1996) [Article in Russian] 6. Chen, W.L., Hwang, J.S., Hu, T.H. et al., 2001. Lenticular opacities in populations exposed to chronic low-dose-rate gamma radiation from radiocontaminated buildings in Taiwan. Radiat. Res. 156, 71-77.
7. Hsieh, W.A., Lin, I.F., Chang, W.P., et al., 2010. Lens opacities in young individuals long after exposure to protracted low-dose-rate gamma radiation in 60Co- contaminated buildings in Taiwan. Radiat. Res. 173, 197-204.
8. Hall, P., Granath, F., Lundell, M., et al., 1999. Lenticular opacities in individuals exposed 7237 to ionizing radiation in infancy. Radiat. Res. 152, 190-195
9. SSK, Radiation-induced cataracts, Recommendations of the Commission on Radiological Protection with scientific reasoning, SSK, Bonn, 2009
10. Wilde, G. and Sjostrand, J., 1997. A clinical study of radiation cataract formation in adult life following gamma irradiation of the lens in early childhood. Br. J. Ophthalmol. 81, 261-266.
11. Choshi, K., Takaku H., Mishima et al. 1983. Ophthalmologic changes related to radiation exposure and age in the adult health study sample, Hiroshima and Nagasaki. Radiat. Res., 96(3), 560-579
12. Otake M, Finch SC, Choshi K. et al, 1992. Radiation-related ophthalmological changes and aging among Hiroshima and Nagasaki A-bomb survivors: a reanalysis. Radiat Res.131 (3): 315-24.
13. Nakashima, E., Neriishi, K., Minamoto, A., 2006. A reanalysis of atomic-bomb cataract data, 2000-2002: a threshold analysis. Health Phys. 90, 154-160.
14. Neriishi K, Nakashima E, Akahoshi M, Hida A, Grant EJ, Masunari N, Funamoto S, Minamoto A, Fujiwara S, Shore RE., 2012. Radiation dose and cataract surgery incidence in atomic bomb survivors, 1986-2005. Radiology 265(1):167-74. Epub 2012 Aug 8.
15. Ainsbury EA, Bouffler SD, Dörr W, Graw J, Muirhead CR, Edwards AA, Cooper J, 2009. Radiation cataractogenesis: a review of recent studies. Radiat. Res. 172, 1-9.
page 17
16. Shore, R. E., Neriishi, J. and Nakashima, E. 2010. Epidemiological Studies of Cataract Risk at Low to Moderate Radiation Doses:(Not) Seeing is Believing. Radiat. Res. 174, 889–894.
17. Michel M, Jacob S, Roger G, Pelosse B, Laurier D, Le Pointe HD, Bernier MO. 2012. Eye lens radiation exposure and repeated head CT scans: A problem to keep in mind. Eur J Radiol. 81 (8): 1896-1900
18. Thorne MC, 2012. Regulating exposure of the lens of the eye to ionising radiations. J. Radiol. Prot. 32, 147–154
19. ICRP, 2012 ICRP Statement on Tissue Reactions / Early and Late Effects of Radiation in Normal Tissues and Organs – Threshold Doses for Tissue Reactions in a Radiation Protection Context. ICRP Publication 118. Ann. ICRP 41(1/2)” http://ec.europa.eu/energy/nuclear/radiation_protection/doc/art31/2012_11_report_goe.pdf (bold added for emphasis)
Note [1]: This case is said to be cataracts cause by congenital rubella (measles), but radiation also causes cataracts.

